Like most patients, cancer survivors want to be empowered to take care of themselves and remain healthy. Once cancer treatment ends, there are some questions every patient should be asking their doctor to be informed about their care and to know what they can expect next. These include, but are not limited to the following:
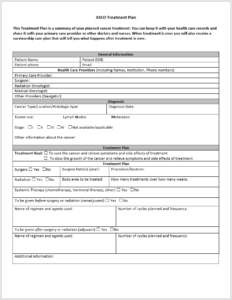
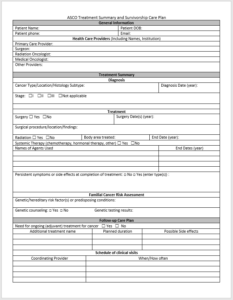
“What treatments and drugs have I been given?”
Patients should require their doctor to provide a written record detailing the type of cancer they had, the treatments and drugs they received, and the potential side effects of these treatments.
“Do I need to seek follow-up care?”
Patients should be given a written cancer survivorship plan that would detail what kinds of screening or tests they should be receiving post-treatment and a schedule of when they should be following up with their primary care or oncology provider to have these performed.
“Will I get cancer again?”
Oncology providers should explain, both verbally and in writing, the risks of secondary cancers or recurrent cancers and what signs or symptoms to look for.
“What should I do to maintain my health and well-being?”
Patients should be advised on the benefits of healthy diets and routine exercise and the perils of not routinely using sunscreen or continuing to smoke. Patients also should ask their doctors, if appropriate, about whether they should inform close relatives about their increased risk of cancer and need for cancer screening.
“Even though I survived cancer, will I feel differently physically?”
Cancer treatment has a different effect on everyone, and for some survivors, there are serious side effects from treatment. Providers need to educate patients and make them aware of the possible short and long term effect that may arise. Radiation could affect a person’s heart, stamina, or fertility. Patients may feel overly anxious or depressed about the possibility of getting cancer again. You should ask your doctor how treatment could affect your long-term health and mental functioning.
“Will I have trouble getting health insurance or keeping a job because of my cancer?”
Having cancer can affect access to health or life insurance, the ability to keep a job, as well as job mobility. Providers should be prepared to offer cancer patients information about what resources are available if they face employment discrimination or are unable to access or keep health and life insurance.
“Are there support groups I can turn to?”
Your provider should be able to provide a useful list of community or nationally based cancer-related organizations or other groups that can offer support with or information on survivorship issues and challenges.
“Now that I’ve finished treatment, who on the cancer team will be responsible for monitoring my care?”
Patients should know who will be the main point of contact working with their primary care provider to coordinate follow-up care related to their cancer treatment.